Africa Must Lead the Fight Against Antimicrobial Resistance Through Hospital-based Antimicrobial Stewardship Initiatives
Antimicrobial resistance (AMR) is a growing global health threat, but its impact is particularly severe in Africa, where resistance infection rates and death are highest.

Published
Author
Share
Editors’ note: In his blog post, Ibrahim Kamara — a former Inter-CeBIL visiting fellow and a medical doctor, public health specialist, and research scientist — explains why Africa must take the lead in combating antimicrobial resistance (AMR) through hospital-based antimicrobial stewardship initiatives. This contribution relates to Inter-CeBIL’s Key Area 2 on Pandemic Preparedness and AMR, with a particular focus on perspectives from the Global South.
Antimicrobial resistance (AMR) is a growing global health threat, but its impact is particularly severe in Africa, where resistance infection rates and death are highest.
In 2021 alone, there were 4.7 million deaths associated with AMR globally, with most of these deaths occurring in Africa, especially in West African countries, including Sierra Leone. Projections indicate that more than 39 million people around the world could die from antibiotic-resistant infections over the next 25 years.
Even though AMR occurs naturally, the inappropriate use of antimicrobials, especially antibiotics, is the primary driver of AMR. To mitigate this societal menace, the World Health Organization (WHO) developed the global action plan (GAP) to combat AMR as a blueprint for countries to develop their national action plans (NAPs). As of 2024, 45 of the 47 countries in the WHO African region had developed their NAPs, and 33 were endorsed by their governments. There’s still much room for improvement in terms of implementation and monitoring, though.
One key objective of these NAPs is to promote the rational use of antimicrobials. Given Africa’s high burden of infectious diseases, widespread antibiotic misuse, and weak healthcare systems, there’s an urgent need for hospital-based Antimicrobial Stewardship Programmes (ASPs). These programs promote the responsible use of antibiotics, enhance patient safety, and reduce healthcare costs. ASPs integrate various interventions, including (i) training of healthcare workers, (ii) monitoring of antibiotic use, (iii) prescription audits, (iv) treatment guidelines enforcement, (v) awareness campaigns, and (vi) infection prevention and control (IPC) measures.
With Africa bearing the brunt of high AMR illnesses and deaths, a multisectoral collaboration is mandatory to fast-track the implementation of ASPs and sustain long-term antimicrobial effectiveness for the treatment of bacterial and other infections. This collaboration must include stakeholders from African governments across ministries concerned with human health, livestock, and the environment; the WHO; health workers, public health professionals, and health system researchers.
Additionally, to succeed, each ASP must be context-specific, tailored to the needs of the different health facility levels, because a ‘one size fits all’ approach for ASP establishment is not pragmatic. I recommend a minimum standard for the ASP at each level of health service delivery, such as having a focal point or an antimicrobial stewardship (AMS) team, depending on the facility type. The higher-level facilities should have multidisciplinary AMS teams comprising an infectious disease specialist (or medical doctor), a pharmacist (or pharmacy technician), a trained nurse, and any other healthcare workers interested in AMS. These AMS focal persons/ teams are responsible for the day-to-day implementation of AMS activities.
Furthermore, a hospital technical committee should be established with a clear mandate that encompasses oversight and supportive supervision, resource mobilization, advocacy, and incentivization to galvanize the AMS interventions and optimize their effectiveness. By applying context-specific, cost-effective AMS interventions, Africa will be better positioned to win the fight against AMR, as the burden and deaths are higher in the region as compared to other parts of the world.
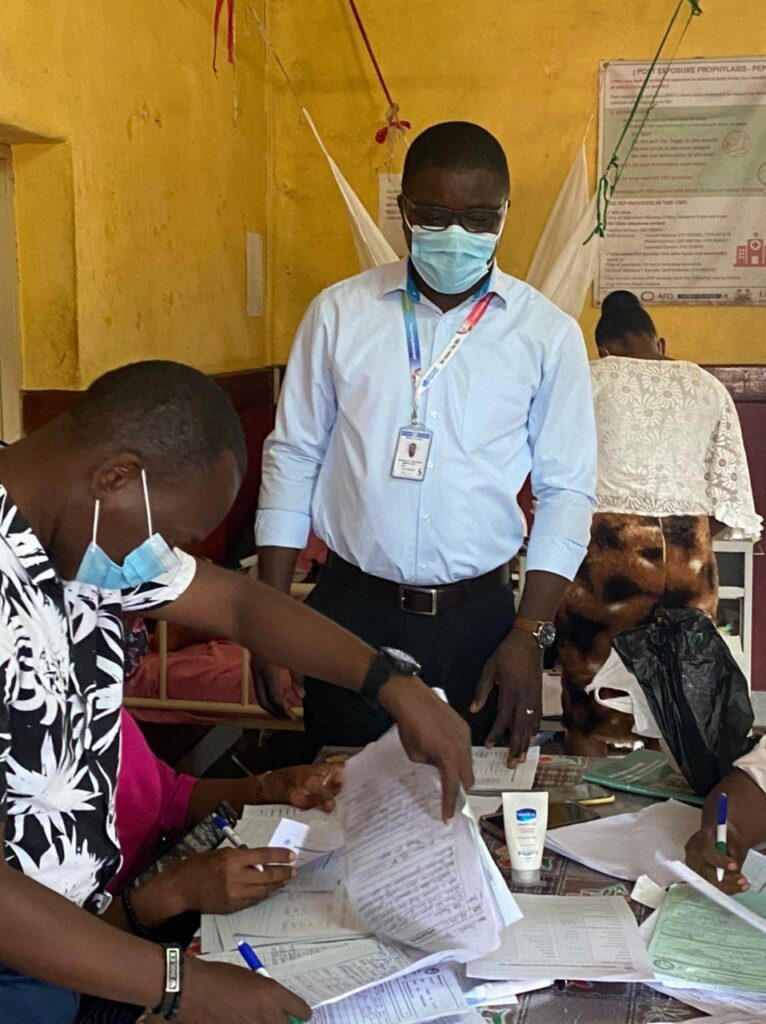
Because of the higher propensity for infections in African countries, ASP should give greater emphasis to hospital IPC activities. Effective IPC practices will ensure a safe environment for patients, their relatives, and healthcare workers. Simple measures like hand hygiene practices, proper waste management, access to safe water and clean sanitation facilities, well-ventilated wards with appropriate bed spacing, and a clean environment will reduce the spread of resistant infections and promote good patient outcomes. “An infection prevented is an antibiotic prescription postponed and an avoidance of likely inappropriate antimicrobial use.”
Research is instrumental for effective ASP implementation. Operational research can be implemented by African researchers to test the standard ASP initiatives and expand the evidence on what works best within the local contexts. This research can be conducted through global south and global north collaboration to ensure shared learning, as there is limited evidence on the effectiveness of the different AMS interventions in diverse contexts.
It is time for Africa to assert its presence in the conversations around AMR through the generation of local evidence and local solutions to this silent pandemic. Africa should engage on the global stage as an equal stakeholder, sharing learnings with the other regions. Africa should rise above the tendency for top-down imposition of solutions for AMR, but instead contribute to the AMR reduction agenda through a win-win approach. This will require African governments to dedicate funding for research to generate local evidence on AMR and AMS. The resultant knowledge exchange will reduce the illnesses and deaths of AMR globally.
We must remember that if Sierra Leone can’t address the problem of resistant infections, Belgium, the United Kingdom, China, the United States of America, and other parts of the world are not safe. We urgently need a collective global campaign to curb this menace to society, and Africa must lead this AMR fight!
This post was originally posted by International Health Policies.
This post is part of a digital symposium called Innovation, Law, and Ethics in International Bioscience. To read the related posts, click here.
Acknowledgment: This article was made possible through the generous support of the Novo Nordisk Foundation (NNF) via a grant for the scientifically independent Collaborative Research Program in Bioscience Innovation Law (Inter-CeBIL Program – Grant No. NNF23SA0087056).